Sepsis is a rare but serious complication resulting from infection. Sepsis is commonly known as septicaemia or blood poisoning. As professionals we now steer away from these terms so you will hear the words sepsis or septic shock.
The medical definition for sepsis is "A life threatening organ dysfunction due to a dyregulated response to infection (JAMA 2016)". What this means is that Sepsis is caused by the abnormal way the body reacts to germs, such as bacteria, entering into your body and developing into an infection.
This results in your body attacking and damaging its own organs and tissues which can lead to septic shock, multiple organ failure and death especially. When sepsis is recognised and treated early with escalation to the appropriate health care teams chances of recovery are vastly increased.
Sepsis can start from any source of infection in the body. This includes lungs (pneumonia), bladder and kidney (urinary tract infections), skin injuries such as cuts and bites (cellulitis), abdomen (such as appendicitis), and other areas (such as meningitis).
Sepsis can be caused by a huge variety of different bugs, many of which are common bacteria which we come into contact with every day without making us ill. Viruses and fungi can also cause sepsis.
It is not known why a common infection develops into sepsis in some people and not others, but we can identify people who are more at risk.
Anyone can develop sepsis but some groups of people are more vulnerable than others. You are more likely to develop Sepsis if you:
- Are very young or very old.
- Are very frail and/or malnourished.
- Have a compromised immune system due to taking drugs to treat cancer (chemotherapy), long term steroids or immunosuppressant drugs.
- Have diabetes.
- Have serious illness which affect your immune system such as AIDS, liver disease or leukaemia.
- Have had an organ transplant and are on anti-rejection drugs.
- Have had a recent surgery, or other invasive procedures.
- Have an infection or complication after surgery.
- Have a wound for example, surgical incision, cuts, burns, blisters or skin infections.
- Are pregnant, have given birth or had a termination or miscarriage in the past 6 weeks.
Sepsis is a complex syndrome which can present like many other illnesses. This can make it difficult to diagnose. However healthcare organisations have recognised this and recently invested a lot of revenue into funding specialist posts and education for front line staff.
There is not a single sign or test for sepsis, but many indications. We teach staff that if your patient is unwell/ sick and this may be due to an infection sepsis must be considered.
You may feel like you are developing a flu-like illness, gastroenteritis or a chest infection at first in the more extreme cases people have reported that they have a feeling of impending doom or that they feel like they are going to die.
In most cases, you will just have an infection so you should contact your GP in the first instance. If you feel there is a decline in health while waiting to be seen or that the case is extreme then dial 111 / 999.
The UK Sepsis Trust provides useful information on how to spot sepsis. They provide support for those who have had sepsis and/or their families and have useful awareness materials.
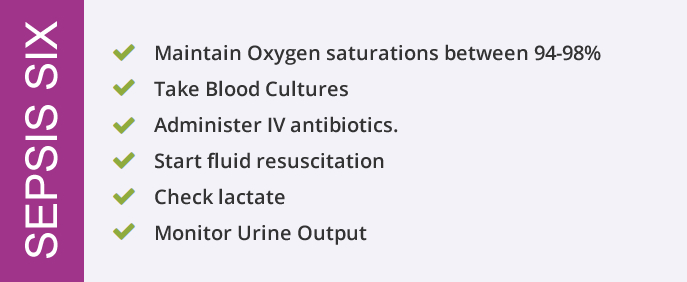
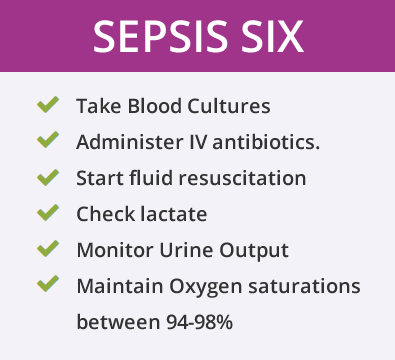
Treating sepsis is time-critical. The UKST recommend a first hour care bundle that should be administered within one hour of sepsis. This bundle is commonly referred to as the Sepsis Six.
Bundles are groups of clinical interventions or treatments that have been proven to be effective in treating conditions such as sepsis when given together.
Sepsis is always caused by infection, most commonly by bacteria. That means that preventing infection is one of the best ways to prevent sepsis.
- Get vaccinated against flu, pneumonia, and any other infections that could lead to sepsis if you are in an at risk group. Talk to your doctor for more information.
- Prevent infections that can lead to sepsis by:
- a. Cleaning scrapes and wound.
- b. Practice good general hygiene and hand washing.
- Following recommended immunisation schedules can reduce the risk of sepsis. Talk to your doctor for more information.
- Stopping the indiscriminate use of antibiotics can help to prevent bacterial resistance to antibiotics. Ensure that you follow your doctor’s instructions for taking antibiotics. Within hospital, your antibiotic regime will be reviewed routinely to ensure you are on the best and most appropriate antibiotic.
How long does it take to recover from Sepsis?
The amount of time it takes to fully recover from sepsis varies, depending on the individual person's overall health and fitness prior to their illness as well as the length and severity of the sepsis. Whilst some people make a full recovery fairly quickly, other people experience long-term physical and/or psychological problems for up to two years afterwards as an effect of being critically ill and spending time in a Critical Care Unit.
Sepsis can cause some additional problems that may not become apparent for several weeks, for example, recurring infections. These long-term problems are known as post-sepsis syndrome (PSS) and can either be physical (e.g. muscle weakness, swollen limbs or changes sensation in limbs) or psychological and emotional (e.g. anxiety or poor concentration)
It is important to remember that not everyone experiences these problems after sepsis and/or being critically ill.
What are the first steps in recovery and rehabilitation?
The purpose of rehabilitation is to restore you back to your previous level of health or as close to it as possible. After you have had sepsis, rehabilitation usually starts in the hospital by slowly helping you to move around and look after yourself. You may need to work with physiotherapists to help you move and do exercises so you can regain your strength. In the event you require more care on discharge this will be assessed whilst you are getting ready to go home.
How will I feel when I get home?
- If you have been seriously ill, it may take time for you to fully recover. You will likely be very tired and will need to sleep and rest a lot, but you might also find sleeping difficult.
- You may feel very weak and lose weight. Simple things, such as getting dressed or even receiving visitors and talking may seem difficult at first as you often feel very tired and need to do more now you are at home. Begin your rehabilitation by building up your activities slowly and rest when you are tired.
- Your skin may be dry, itchy and peel. A skin moisturiser may help. Your nails might break easily and your hair may change. In extreme cases, people have reported hair loss or thinning.
- You may find that you don’t have an appetite. Build this up by eating small meals several times a day rather than three large meals per day. Nutrition drinks that can be bought in local stores may help.
- It is not unusual to feel anxious, depressed, unmotivated or to experience a lack of enjoyment in things you usually do. You may have difficulty concentrating and feel frustration at not be able to do things you took for granted such as walking or eating. You may become upset or cry for what may seem like no reason. Some people experience flashbacks, nightmares and PTSD (Post Traumatic Stress Disorder).
Generally, these problems do improve with time. They are a normal response to what you have been through. Speak to your GP or healthcare provider about local resources available to help you while you get better.
What can I do to help myself recover at home?
It might help to:
- Set small, achievable goals for yourself each week, such as walking up the stairs.
- Rest and rebuild your strength.
- Talk about what you are feeling to family and friends.
- Keep a journal so you can see that you are getting better and stronger.
- Learn about sepsis to understand what happened.
- Ask your family to fill in any gaps you may have in your memory about what happened to you.
- Eat a balanced diet.
- Exercise if you feel up to it.
- Make a list of questions to ask your doctor when you go for a check up.
You should find it easier to cope as time goes by and as you begin to get stronger and get back to doing your normal activities. If you feel that you are not getting better or are finding it difficult to cope, see your GP for help.
The UK Sepsis Trust also provides information on support for survivors and their relatives as well as for bereaved.
What's normal and when should I be concerned?
Generally, the problems described on this page do improve with time. They are a normal response to what you have been through. However, if you feel that you are not getting better, or finding it difficult to cope, or continue to be exhausted speak with your GP or healthcare provider.



